Dubai: You may have tested negative or positive. It doesn't matter. You should still wear a mask for the foreseable future.
Here's why you should wear a face mask as much as possible.
Q: I’m a recovered COVID-19 patient. Do I need to wear a mask?
Yes. Several studies show why you should keep wearing a mask. So you may be a recovered patient and may no longer have the symptom (asymptomatic). But that doesn’t mean you’re incapable of spreading (or shedding) the virus. There's no evidence of that.
There's the risk of “viral shedding” (transmitting the virus to another person), even if you had already been cleared of infection, or tested negative, studies show.
There’s a build-up of clinical and mathematical modeling studies being done around the world to better understand SARS-CoV-2 viral transmission, especially the asymptomatic type.

One study (pre-print version), conducted by the University of Southern California, suggests that the number of asymptomatic cases and the spread of COVID-19 are much higher than previously thought or modelled.
Another study, set for publication in the upcoming May 1, 2020 edition of The Lancet, shows the "prolonged presence of SARS-CoV-2 viral RNA in faecal samples".
These are important bits of information health authorities and policy makers will consider.
Examples of human diseases caused by RNA viruses include the common cold, influenza, SARS, COVID-19, hepatitis C, hepatitis E, West Nile fever, Ebola virus disease, rabies, polio and measles.
Q: For how long should I wear a mask?
It’s not clear. It's up to the health authorities to declare when not wearing a mask would be a safe thing to do, especially when outside.
Until now, scientific studies remain inconclusive on how long is the “viral shedding” of SARS-CoV2. For those who are immuno-compromised (i.e. with pre-existing conditions), the deadly virus — reportedly having already mutated into several variants — remains a clear, possibly fatal threat.
There’s no specific vaccine or medicine for SARS-CoV-2 yet. So while the world's top scientists try to get the full pathogenicity of this virus (how long does it actually survive in surfaces or water, for example?), and come up with a vaccine that's both safe and effective, it's best to take extra care.
A lab in Paris detected "minuscule traces" of coronavirus in non-potable water used for cleaning.
And because the virus is new, the disease tolerance mechanism encoded in the human defences essential for survival after an infection is also little understood.
One study, done by a German team, shows people who contract the novel coronavirus emit high amounts of virus very early on in their infection. At the same time, the Germans found that people with mild infections can still test positive by throat swabs for days and even weeks after their illness. The researchers, however, found that those who are only mildly sick are likely no longer infectious by about 10 days after they start to experience symptoms.

Going forward, these are important bits of information health authorities and policy makers will consider in the protocols to be adopted when in public places — or when flying.

What’s clear is that at peak shedding, people with COVID-19 emit more than 1,000 more virus than was emitted during peak shedding of SARS infection — a fact that likely explains the rapid, dangerous spread of the novel coronavirus.
Virulent describes both disease severity or a pathogen's infectivity.
Q: Why should I take extra care, and wear a mask whenever I'm out?
First, if you’re in the UAE, you could get slapped a Dh1,000 fine when outside your house without a face mask.
Second, as stated above, not much is understood about the SARS-CoV-2 pandemic and its reported viral mutations.
Another study reports that the coronavirus has mutated into at least 30 variants. It is yet unknown what mechanism of virulence (MOV) each variant carries.
Moreover, cases have been reported where a patient could infect their close contacts even after “apparent recovery” from the infection.
Scientists all over the world are feverishly contributing to the increasing body of knowledge of the novel coronavirus.
In another report, published in The New England Journal of Medicine, a laser light-scattering experiment visualised speech-generated droplets and their trajectories. The study concluded that droplets expelled from a speaker’s mouth decreased in instances of speech at a lower volume — and were almost eliminated when the speaker’s mouth was covered with a damp cloth.
Yet, despite these numerous studies, the “viral shedding” window of SARS-CoV-2 has not been completely understood, says the CDC.

Q: What’s the significance of these studies?
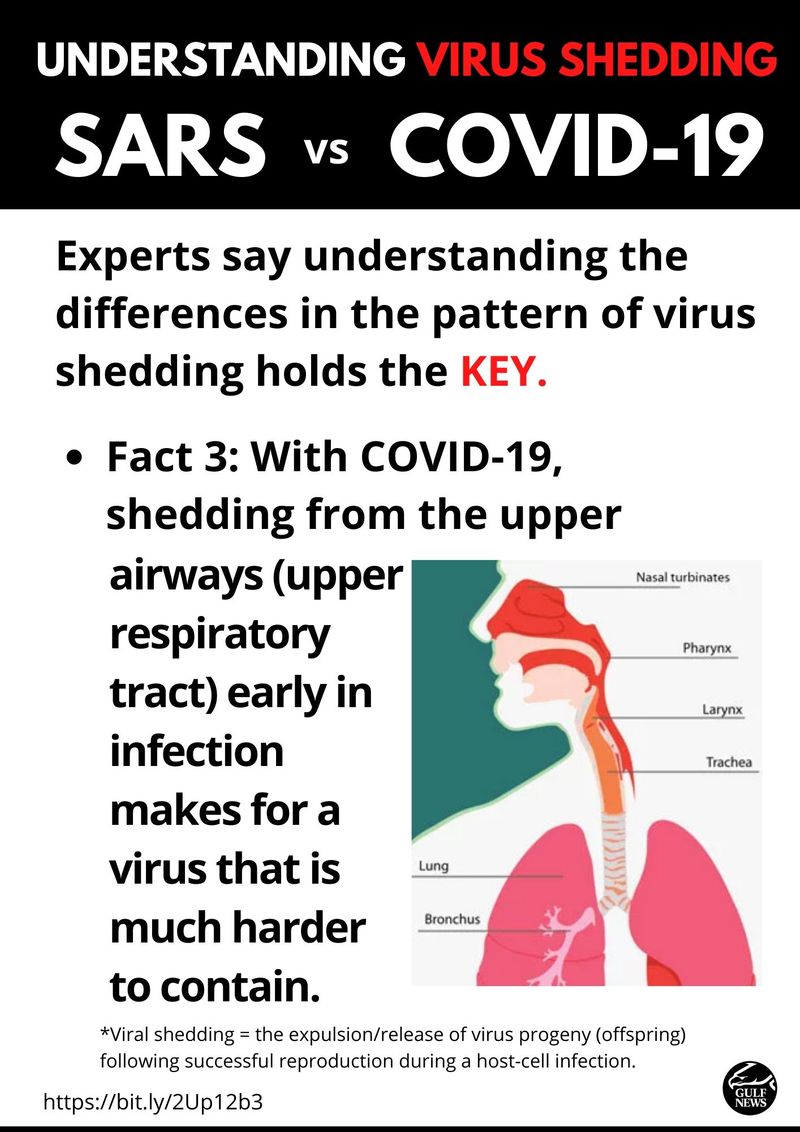
In the second, published by JAMA and conducted in Singapore involving the first 18 patients (who all survived) diagnosed with SARS-CoV-2 in the island-nation (between January 23 and February 3, 2020), the researchers described all the patients having tested positive for respiratory tract infection.
The Singapore team found prolonged “viral shedding” from the nasopharynx of 7 days or longer in 15 patients. This meant 83% of them were shedding the virus for at least 7 days. The Singapore study was conducted on patients with milder infections that recovered from the disease.
Still, researchers warned: “It is currently unclear if there is a delayed viral clearance in the more vulnerable population such as those older or have immune deficiencies or are on immunosuppressive therapies.”
In another study, published by Chinese and US clinicians in The Lancet, the authors found that virus persisted for 20 days, though the patients studied had a high mortality of >40%.

Q: Why is this piece of information important?
Research has established that SARS-CoV-2 can transmit from "subclinical" patients, i.e. that patients who are considered "recovered" are still able to spread the virus. It continues to pose a threat for those who are immuno-compromised (people with lower levels of immunity due to pre-existing condition, i.e. diabetes, cardiovascular issues).
The increasing body of scientific data about SARS-CoV-2 can also be a useful tool for everyone, medical workers and policymakers, especially.
As we all know, the current COVID-19 is a pandemic. It has surpassed both MERS and SARS in severity and deaths within a rather short period.
This illness has, without a doubt, already changed the world as we know it.
It's clear that aside from taking other necessary COVID-19 precautions, such as proper hand washing and disinfection, wearing a mask when in public is the least we can do. The face mask is a new reality this unseen enemy has forced upon us.