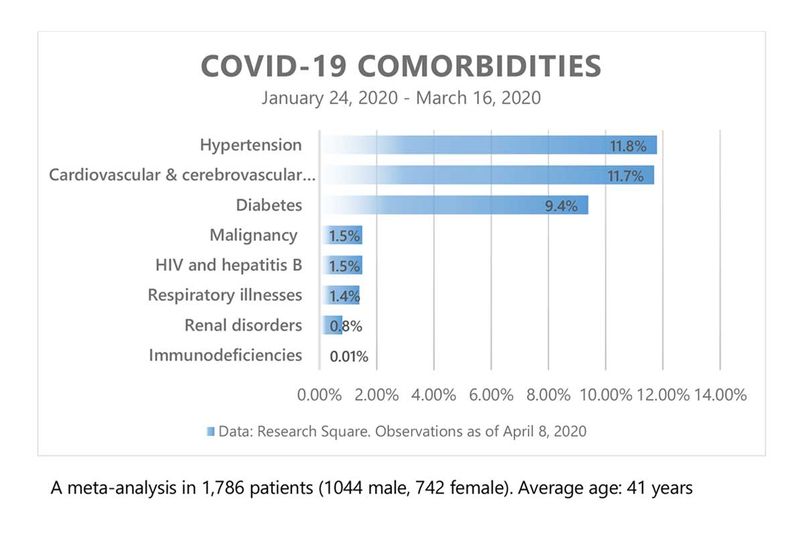
If you have diabetes, a COVID-19 attack could severely impact your health. That’s not new. Diabetes is a known comorbidity –– an underlying condition that could undermine the human immune system’s ability to fight the new coronavirus.
What’s new is the elevated levels of sugar in the blood of COVID-19 patients who do not have diabetes. Most of these cases have been reported from India. Public hospitals in Mumbai have reported cases of patients with hyperglycemia (high levels of sugar in the blood) with readings of around 400-500 mg/dL. (A blood sugar level of under 140 mg/dL is considered normal).
Some of these patients are very young, around 25 years. Many of them don’t have a history of diabetes: they are neither prediabetic nor have undiagnosed diabetes.
Typically diseases, infection, injury or stress can result in high levels of sugar in the blood. But a sugar surge in non-diabetic COVID-19 patients is unusual, Mumbai Mirror quoted Dr Jeenam Shah, a pulmonologist, as saying.
COVID-19 is primarily a respiratory disease, where the coronavirus attacks the lungs. But other complications include damage to the tissues in the liver, kidney, intestines and heart, leading to organ failure. Blood clots and additional viral and bacterial infections, injuries to the brain and central nervous system have also been reported.
More than six months have elapsed since the virus, named SARS-CoV2, surfaced in Wuhan, China. It has since spread to more than 216 countries and territories, and infected more than 12 million people. Even today, after more than 555,000 deaths, the full extent of the health issues caused by the virus is still not known. With each day, more complications are being reported.
Not everyone is at risk of developing complications from COVID-19. Underlying medical conditions increase the risk of complications, and diabetes is one of them.
What’s diabetes?
Diabetes is a condition when the body fails to produce enough insulin to process the sugar in the bloodstream. Insulin, a hormone produced by the pancreas, helps move sugar or glucose from the blood into the cells of the body.
The body breaks down carbohydrates from food into sugar (glucose), which is absorbed into the bloodstream. And glucose is required for cells in the body to produce energy. Lack of insulin to transport glucose into the cells results in lethargy (lack of energy) and leads to other complications.
With insulin therapy and other treatments, people with diabetes can manage the condition and live healthy lives.
Three types of diabetes
Type 1 diabetes: In this case, the body does not produce insulin, hence the name insulin-dependent diabetes. It used to be referred to as juvenile diabetes as the condition usually appears in childhood or adolescence, but adults can also develop Type 1 diabetes.
There’s no cure for the condition, believed to be caused but genetic factors and some viruses. Treatment generally focuses on managing blood sugar levels with insulin, and through diet and lifestyle.
Type 2 diabetes: This is the most common form of diabetes, where the body either doesn’t produce sufficient insulin or the insulin produced is not used correctly. When there’s not enough insulin to move the sugar from the blood into the cells of the body, sugar levels in the blood rise dramatically.
This condition can be managed very well with changes in lifestyle, mainly diet and exercise. Acute cases will require medication.
Gestational diabetes: It occurs when blood sugar levels become high during pregnancy. Gestational diabetes tends to go away after childbirth, but it increases the risk of Type 2 diabetes later. Class A1 gestational diabetes can be managed through diet and exercise, but women with class A2 gestational diabetes will need medications.
What are the symptoms of diabetes?
The general symptoms described in WebMD include increased thirst; feeling hungry very often; frequent urination; unexplained weight loss; fatigue; blurred vision; headaches; red and swollen gums; slow healing of infections; tingling sensation in hands and feet, and loss of consciousness.
There are a host of complications arising from diabetes, and that include hypoglycemia (blood sugar level falls below 70mg/dL), hyperglycemia (blood sugar level rises above 180-200 mg/dL), nerve damage, glaucoma and many others.
Why diabetics are vulnerable to COVID-19
People with diabetes lack a robust immune system to fight the new coronavirus. Decreased insulin output impacts immunity and makes the body susceptible to infections and other chronic health issues.
People with diabetes tend to have less than average blood flow, making it difficult for the body to transport nutrients to protect against infections and help in the healing process. Diabetes also keeps the body in a low-level state of inflammation, so the healing response to any infection will be slower, says Medical Science Today.
High blood sugar levels and a persistent state of inflammation makes it difficult for people with diabetes to recover from illnesses like COVID-19.
How coronavirus attacks the body
When a person inhales virus-laden droplets, SARS-CoV-2 enters the nose and throat. The nose lining is rich in the angiotensin converting enzyme 2 (ACE2), which usually helps in regulating blood pressure. The ACE2 is the doorway for the coronavirus to enter a cell. The virus infects a cell by attaching to its surface through the receptor ACE2. This is facilitated by the sugar coating on both the ACE2 and the virus.
Once inside the cell, the virus hijacks the cell functions and uses it to replicate swiftly. The newer copies go on to invade more cells. At this point, if the immune system is unable to subdue the virus, it moves through the windpipe into the lungs.
The patient’s condition deteriorates as lung tissues are teeming with ACE2, and that makes it the favoured location (some call it Ground Zero) for the coronavirus to launch attacks. At this point, the situation may become critical, and the infections may trigger a cytokine storm (an overreaction from the body’s immune system that can be fatal).

ACE2 is also found in the pancreas and other organs, but not as densely as in the lungs.
Adam M. Brufsky, professor of medicine, University of Pittsburgh, argues in the Journal of Medical Virology that the severity of COVID-19 infection is influenced by the concentration of the sugar-coating on the virus and the ACE2 receptors in the lung tissues. So high blood sugar not only increases the number of ACE2 receptors in the lungs but also provides an increased concentration in the sugar coating. Ideal conditions for a COVID-19 virus invasion.
How people with diabetes can beat COVID-19
People with diabetes can avoid serious complications from COVID-19 if the sugar levels in the blood are well-managed. Fluctuating blood sugars raises the risk as the body’s ability to fight infections is compromised.
Since COVID-19 is a viral infection, it can increase inflammation, or internal swelling leading to more severe complications.
Why non-diabetic persons get a sugar spike
A sudden increase in sugar level in the blood is the body’s response to inflammations, infections or trauma. It’s a stress response that results in higher-than-normal blood sugar levels, says a report in the Medical Science Today.
So a person’s body needs to produce extra insulin during an illness. But stress blocks the body from releasing insulin, allowing glucose to build up blood. Persistent stress will lead to higher sugar levels.
Why some COVID-19 patients develop temporary diabetes
A viral attack is enough stress for the body to respond with extra sugar output. But in many cases, especially the ones reported from Mumbai, India, the sugar surge in COVID-19 has been temporary. And doctors there are now studying these patients to see whether they develop Type 2 diabetes later in life.
Physicians in the United States have reported that a lot of COVID-19 patients in their hospitals not only had diabetes and prediabetes but others had high blood sugar without being aware of it, writes Brufsky in The Conversation.
This temporary sugar surge had been noticed in SARS (caused by another coronavirus) patients as well, he says.
How coronavirus affects insulin production
Doctors at the civic hospitals in Mumbai insist that the sugar surges in their patients are not cases of undiagnosed diabetes.
Perhaps the observation of Shashank Joshi, an endocrinologist based in Mumbai, holds some clues to this phenomenon. “Not only do patients come in with high glucose levels, they also have elevated pancreatic enzymes,” Joshi told the Times of India.
This may be due to the presence of lots of ACE2 receptors on the islet cells, which make insulin in the pancreas. If a coronavirus infects these cells, they will stop making insulin resulting in temporary diabetes.
Why COVID-19 patients are advised to stay off sugar
When there is more insulin, there is less sugar. That means fewer ACE2 receptors and less sugar on the ACE2 receptors, and this may reduce the chances of a virus entering the cells. This may be the reason why doctors tell COVID-19 patients to avoid sugary foods.